V-254 Wound Lamp Protocols
Purpose
Click here for video about this lamp and research.
The bactericidal UVC light treatment program is an adjunctive therapy for reducing and eliminating bacterial bioburden that can impede wound healing. This method of treatment is consistent with wound care best practice guidelines. It is an important modality for cleaning a wound of surface infection where conventional methods have been ineffective. UVC light is well documented in the medical literature as effective and safe for:
- Combating a developing surface infection
- Infected wounds where poor circulation reduces the effectiveness of systemic antibiotics
- Replacement of topical antibiotics
- Treating antibiotic resistant species such as MRSA
In addition, it has been shown to have beneficial effects for:
- Producing a mild inflammatory response to help accelerate wound healing
- Dermatological conditions where UVC light is indicated
UVC light is not intended as a prophylaxis, or as a replacement for appropriate infection control measures.
The UVC light is applied:
- Directly to the infected wound bed. Periulcer areas are protected carefully with petroleum jelly and draping. Exposure times are 1.5 to 2.5 minutes, typically, to provide the maximal bacteria kill rate, and/or
- To the wound and periulcer areas to produce a light erythema, using shorter exposure times of 15 to 60 seconds, as determined by sensitivity testing. This produces a mild stimulation effect to help elicit a healing response
and to help shorten healing times. UVC light therapy is compatible with any concurrently administered systemic antibiotics.
For cases of deep cellulitis and osteomyelitis that are not responsive to UVC light, additional therapeutic modalities should be used.
UVC light does not produce tanning or burning as does UVA and UVB light.
Contraindications
- Light sensitive disease, such as but not limited to porphyria or lupus erythematous
- Melanoma or history of melanoma
- Invasive squamous cell carcinomas, or history
- HIV
- Fever
- Deep X-ray therapy
Description
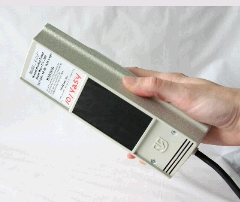
The therapy program is considered medically necessary for patients needing treatment for these conditions. A nurse (RN or RPN) who has received instruction on the use and operation of the UVC light performs the treatment using
theV-254 Wound bactericidal UVC lamp. The nurse, patient and other persons in the vicinity of treatment wear protective UVC blocking eyewear.
Prior to treatment, the nurse performs a sensitivity test for 15 seconds on an unaffected area of the patient’s skin to determine the patient’s response to the UVC light. The nurse or caregiver observes the response in the 24 hours
after exposure. Either no response or a very mild reddening is expected. If the purpose is to produce erythema, the nurse increases the dose each day to the wound area by 15-second increments, if needed, until the desired effect is
achieved.
Therapy is tailored to the patient’s requirements and wound complexity, exposing multiple wound sites sequentially. The starting session will be rescheduled if there are conflicting personal circumstances that would
limit the patient’s commitment to the program. A treatment regimen consists of daily UVC light exposures. Administer ten treatments and then reevaluate. Five treatments are anticipated to produce results. The nurse discontinues treatments when the area is cleared of infection. Excessive pretreatment bioburden and multiple bacteria strains will require a longer treatment program.
The treatments are scheduled to coincide with daily dressing changes, if possible. Where dressings are changed less frequently, such as every 2 – 3 days, the UVC light is applied accordingly, but a longer time will be required to
eradicate the bacteria and produce wound closure. The nurse adjusts the exposure time up or down each day according to the wound response, the patient’s tolerance, and any adverse effects such as excessive erythema or blistering.
The UVC light exposure produces a direct physiological benefit to the affected area. The exposure dose for wound healing is generally 1st and 2nd degree erythema, which corresponds to a minimal reddening though a readily visible reddening. Higher dosage can be prescribed to produce 3rd or 4th degree erythema for specific dermatological applications where destruction and exfoliation of the surface area is desired.
Results
Successful outcomes are expected in most cases. Where healing has been hampered by excess bacterial bioburden, the wound can now be expected to progress to full closure once the bacteria colonization is eliminated.